Exocrine Pancreatic Insufficiency: When Digestion Fails
STEVEN SANDBERG-LEWIS
N.D., DHANP
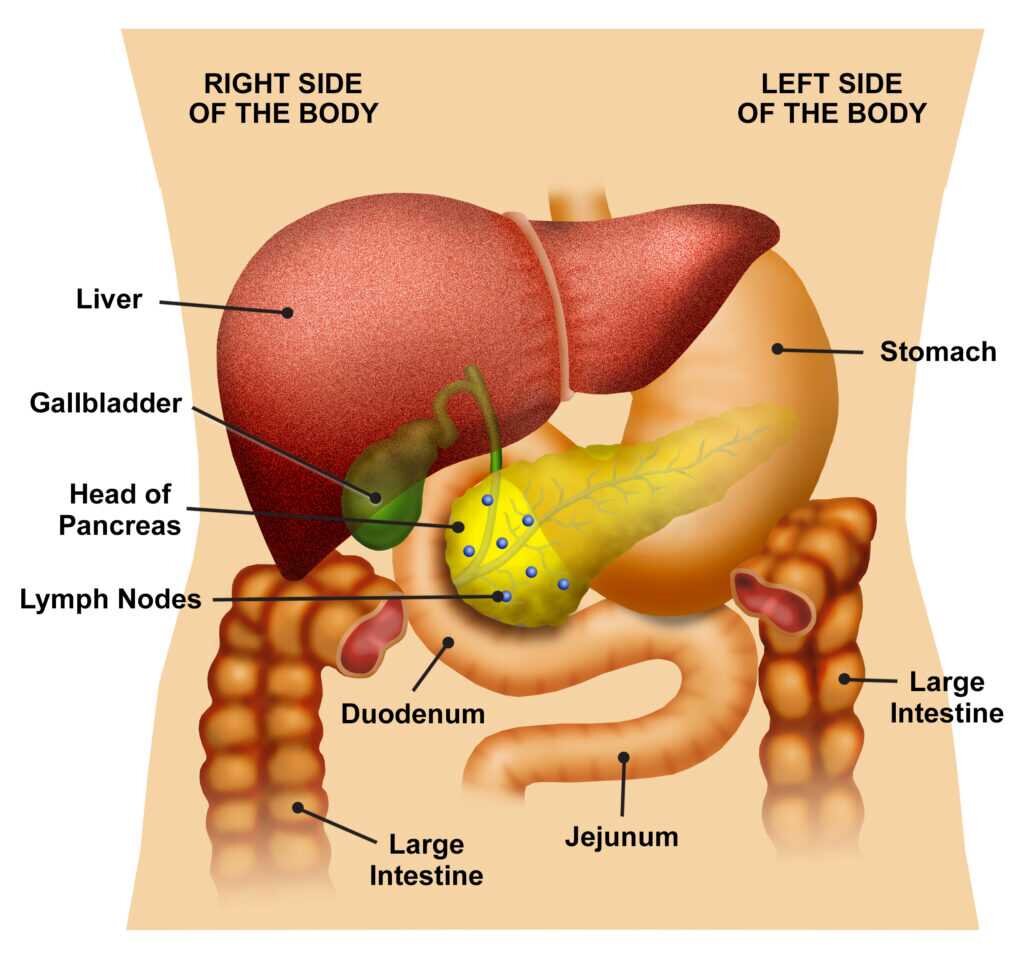
The pancreas is a digestive organ that is tucked beneath the stomach. It has a digestive (exocrine) portion and a hormonal (endocrine) portion. In this article I will focus on the digestive part.
The pancreas is unique among gastrointestinal organs because it produces enzymes that are involved in digesting fats, proteins and carbohydrates. These are made in acini, small exocrine cell-lined areas that drain into ducts that transport the enzymes to the small intestine.
The digestive route prior to the intestine:
Food is chewed and swallowed down the esophagus and enters the stomach within seconds. Here proteins are broken down by acid and an enzyme called pepsin. They are turned into peptides which are short chains of amino acids. There is essentially no digestion of fats or carbohydrates here. Over 4-5 hours, the food gradually leaves the stomach to enter the first part of the small intestine, the duodenum.
There is a lot going on in the duodenum and much of it is done by the pancreas. The pancreas releases its various fluids into the duodenum. First, the acid from the stomach must be neutralized in order to prevent duodenal ulcers. The pancreas releases bicarbonate which quickly changes the pH from a strong acid to a very weak acid. Mammalian pancreatic enzymes are inactive in highly acid solutions, so the bicarb is also needed for the enzymes to function.
The pancreas produces many enzymes. These include trypsin and chymotrypsin for protein digestion, amylase for carbohydrate digestion, lipase for fat digestion and elastase for the breakdown of connective tissue such as tendons and ligaments. Stool levels of elastase and chymotrypsin are the tests used to determine pancreatic digestive function. When stool elastase levels are below 200 ug/mL, a diagnosis of pancreatic exocrine insufficiency is made. Fun fact – elastase is an enzyme unique to the human pancreas.
Exocrine pancreatic insufficiency (EPI or PEI)
Diseases that may be underlying causes for EPI include cystic fibrosis, types I and II diabetes mellitus, chronic pancreatitis, chronic viral hepatitis, short bowel syndrome, hemochromatosis, partial surgical removal of the stomach or pancreas, pancreatic cancer and celiac disease. I also diagnose EPI in patients who have none of these serious conditions, but rather have intestinal bacterial overgrowth, hypochlorhydria (low production of stomach acid), adrenal gland imbalances or biliary sludge (thick bile that does not flow readily through the bile ducts.) Hormone imbalances of estrogen, cortisol or testosterone may also cause EPI.
Typical symptoms and signs of pancreatic enzyme insufficiency include chronic diarrhea, weight loss, inability to gain weight and malabsorption of nutrients leading to high levels of undigested fat in the stool. The classic stool is called steatorrhea – meaning fat flows through. If this goes on long enough it can cause nerve, skin, blood, bone and hormonal problems due to deficiencies of the fat-soluble vitamins A, D, E and K as well as essential fatty acids. Of course, protein and carbohydrates will also be mal-absorbed to a greater or lesser extent.
Luckily, just as in type 1 diabetes mellitus – which can be treated with insulin replacement since it is a deficiency of the hormone insulin – pancreatic exocrine insufficiency can be treated by replacing the deficient enzymes.
There are several forms of these enzymes:
1) “Plant” enzymes – These are actually derived from Aspergillus, a fungus, although they contain no mold, yeast or fungus. They function in a very wide pH range, from about 2 to 12 (very acid to very alkaline). For this reason, they can start working in the stomach and may be especially effective for people who make too little or too much stomach acid. They work best if taken before meals.
2) Animal derived enzymes – These are derived from pork pancreas. They do not start working until the stomach contents empty into the duodenum. They can only function in the narrow pH found there which is close to the neutral pH of 7. They are generally referred to as pancreatin and pancrealipase. They work best when taken at the end of meals.
3) Prescription enzymes – These are also derived from pork pancreas but are enterically coated so that the capsules do not dissolve until they leave the stomach. Unfortunately, the enteric coating may contain phthalates and polyethylene glycol which may be problematic. Other enteric coatings contain talc or carnauba wax and carrageenan, methacrylic acid ethyl acrylate copolymer or polyvinylpyrrolidone (a water soluble plastic).
4) A fourth group of digestive enzymes are the brush border enzymes. These are not actually pancreatic enzymes but are sometimes added to plant enzymes to increase their effectiveness. They are produced on the tips of the lining cells of the intestinal mucous membrane and fine tune the last stages of carbohydrate digestion after the pancreatic enzymes have done their job. The brush border enzymes have names such as sucrase, maltase, lactase and glucoamylase.
It may be difficult to compare the various formulations of pancreatic enzymes. Unfortunately, there are multiple systems for measuring these ingredients and often you will see different systems among the ingredients in any one product. Examples are AGU, HUT, USP, DU, PC, FIP, etc. For this reason, if you have been diagnosed with EPI, I strongly suggest methodically trying various pancreatic enzyme formulations and in various dosages until finding one that makes a significant difference in stools, digestive comfort and overall nutritional absorption. Don’t give up if the first one tried does not prove helpful. It is essential to continue until the right one is found.
Steven Sandberg-Lewis, ND, DHANP, has been in clinical practice for 44 years, with a focus on functional gastroenterology. He has been a professor since 1985, teaching a variety of courses but primarily focusing on gastroenterology and GI physical medicine. In 2019, Dr. Sandberg-Lewis co-founded Hive Mind Medicine, continuing his specialization in gastroenterology with a focus on reflux, SIBO, inflammatory bowel disease and functional GI disorders. He is currently working on his latest book, Let's Be Real About Reflux: Getting to the Heart of Heartburn, written to help non-medical and medical professionals alike develop a better understanding of diseases affecting the gastrointestinal tract.
Hive Mind Medicine blog posts are for educational purposes only and are not intended as medical advice. Please consult with your health care practitioner for personalized guidance. Click on the contact button below if you would like to schedule with one of our Hive Mind practitioners.